Autoimmune disorders affect millions of people worldwide and often develop gradually, making them difficult to recognize in the early stages. One of the most common autoimmune conditions affecting the endocrine system is Hashimoto Thyroiditis, a disorder that directly impacts thyroid function and overall metabolic health. Although it progresses slowly, early awareness and proper management can significantly improve quality of life.
What Is Hashimoto Thyroiditis?
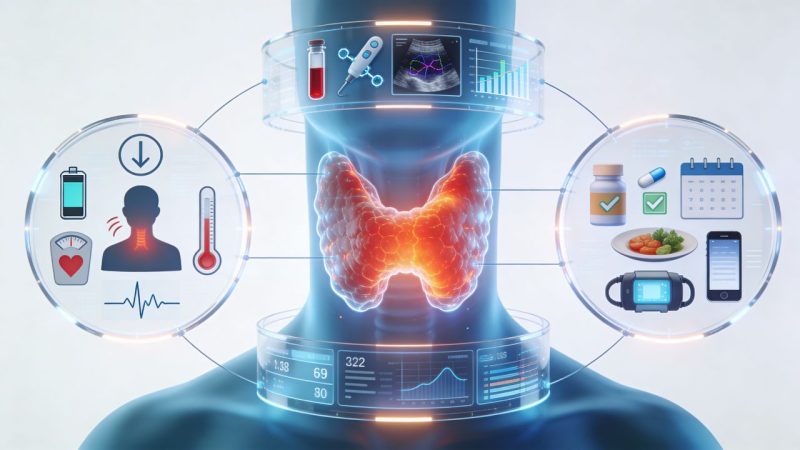
Hashimoto Thyroiditis is an autoimmune disease in which the immune system mistakenly attacks the thyroid gland. The thyroid is a small, butterfly-shaped gland located at the front of the neck and plays a crucial role in regulating metabolism, energy levels, body temperature, and hormone balance.
Over time, the immune attack damages thyroid tissue, reducing the gland’s ability to produce essential hormones. This often leads to hypothyroidism, a condition characterized by an underactive thyroid.
Hashimoto Thyroiditis is more common in women than men and often develops between the ages of 30 and 50, although it can occur at any age.
Common Symptoms and Early Warning Signs
Symptoms of Hashimoto Thyroiditis can be subtle at first and may be mistaken for stress, aging, or lifestyle-related fatigue. As thyroid hormone levels decline, symptoms typically become more noticeable and may include:
- Persistent fatigue and low energy
- Unexplained weight gain
- Sensitivity to cold
- Dry skin and hair thinning
- Constipation
- Depression or mood changes
- Memory and concentration difficulties
- Swelling in the neck (goiter)
Because these symptoms can overlap with other conditions, many individuals remain undiagnosed for years.
Why the Thyroid Matters So Much
The thyroid gland influences nearly every organ system in the body. When thyroid hormone production is disrupted, metabolic processes slow down, affecting digestion, heart rate, mental clarity, and even reproductive health.
In Hashimoto Thyroiditis, the gradual destruction of thyroid tissue can make hormone levels unpredictable. Some patients experience periods of normal thyroid function before hypothyroidism becomes permanent, which is why regular monitoring is essential.
Causes and Risk Factors
The exact cause of Hashimoto Thyroiditis is not fully understood, but several factors are believed to increase the risk:
- Genetics: A family history of autoimmune disorders
- Hormonal factors: Higher prevalence in women
- Environmental triggers: Excess iodine intake, infections, or chronic stress
- Other autoimmune conditions: Such as type 1 diabetes or rheumatoid arthritis
These factors may combine to trigger an abnormal immune response against the thyroid gland.
Diagnosis and Medical Evaluation
Diagnosing Hashimoto Thyroiditis typically involves a combination of clinical evaluation, blood tests, and sometimes imaging studies. Blood tests are used to measure thyroid hormone levels (TSH, T3, and T4) as well as thyroid antibodies, particularly thyroid peroxidase (TPO) antibodies.
An ultrasound of the thyroid may be recommended to assess inflammation or structural changes in the gland. Early diagnosis allows healthcare providers to begin monitoring hormone levels and initiate treatment when necessary.
For detailed medical insight and treatment options, reliable clinical resources such as
Hashimoto Thyroiditis provide comprehensive information on diagnosis and care.
Treatment and Long-Term Management
There is currently no cure for Hashimoto Thyroiditis, but the condition is highly manageable. Treatment primarily focuses on replacing missing thyroid hormones through medication. Levothyroxine, a synthetic form of thyroid hormone, is commonly prescribed to restore normal hormone levels.
With proper dosage and regular follow-ups, most individuals can lead normal, active lives. Treatment is usually lifelong, and medication adjustments may be required over time based on blood test results and symptom changes.
Lifestyle Considerations and Supportive Care
In addition to medical treatment, lifestyle choices can support thyroid health and overall well-being. Balanced nutrition, stress management, adequate sleep, and regular physical activity all play a role in symptom management.
Some individuals benefit from monitoring iodine intake and addressing nutrient deficiencies such as selenium, iron, or vitamin D under medical supervision. However, dietary supplements should never replace prescribed treatment and should only be used with professional guidance.
Living Well With Hashimoto Thyroiditis
A diagnosis of Hashimoto Thyroiditis can feel overwhelming, but understanding the condition empowers patients to take an active role in their health. Regular medical checkups, medication adherence, and awareness of symptoms help prevent complications and improve long-term outcomes.
Education and early intervention are key. When properly managed, most people with Hashimoto Thyroiditis maintain stable hormone levels and enjoy a good quality of life.
Conclusion
Hashimoto Thyroiditis is a common yet often underdiagnosed autoimmune condition that affects thyroid function and overall health. Recognizing symptoms early and seeking medical evaluation can make a significant difference in long-term management.
With accurate diagnosis, appropriate treatment, and ongoing care, individuals can effectively manage the condition and maintain physical and emotional well-being. Understanding the thyroid’s role is the first step toward taking control of thyroid health.
